

Our gut is a wonderful ecosystem with over 100 trillion bacteria making up a large community that works with each other and with our immune system to keep us safe and functioning well.
This microbial community is called our gut microbiome. Irritable bowel syndrome is called a functional gut disorder, because medical tests generally all come back normal but there is still an issue with the way the gut is functioning. This is usually associated with a change in the balance of the gut ecosystem.
The gut microbiome is different in IBS than non-IBS individuals, this is called dysbiosis. The chemical messages created by this imbalanced gut microbiome can affect how quickly the large bowel moves leading to constipation and/or diarrhea as well as altering pain signals to our brain.
Irritable bowel syndrome
is defined as a chronic functional gut disorder and symptoms can include pain, bloating, excess gas and disordered bowel habits, with both unpredictable form and frequency of bowel movements.
IBtrol was developed to
address the symptoms of IBS
but also the underlying dysbiosis of the gut microbiome, helping to foster a balanced gut ecosystem while also managing symptoms of pain, excess gas production and unpredictable bowel movements.
Dr Bridgette Wilson has worked with Medtrition
in the development of IBtrol and with almost two decades of clinical and research experience in IBS, Dr Wilson has ensured that IBtrol is right for all types of IBS. IBtrol includes 3 potent evidence-based components, premium blonde psyllium, GOS-prebiotic and a 5-strain probiotic all at IBS specific doses.

Psyllium
A review of supplements for IBS published in 2020 (Dimidi et al, 2020) found that psyllium improves both abdominal pain and overall symptoms of IBS. A review published in Nature Medicine found that psyllium is useful for normalizing bowel movements in people with IBS with either diarrhea or constipation (Gill et al 2021). Psyllium fiber doesn’t lead to excess gas production when consumed with water, it helps to bulk stool and it binds excess fluid in the gut, making it useful for the treatment of both constipation and diarrhea without worsening IBS symptoms (So et al 2021). 10g of psyllium per day is recommended to see the benefits in IBS.
Prebiotic
Our patented beta-galacto-oligosaccharide (b-GOS) prebiotic is the most extensively researched prebiotic in functional bowel disorders. It has been demonstrated to improve symptoms of IBS in four human clinical trials (Silk et al 2009, Wilson et al 2020, Vulevic et al 2019, Huaman et al 2018). The dose that we have included in IBtrol showed the best effects on IBS symptoms (1.4g of b-GOS per day).


Probiotic
IBtrol combines 5 potent strains of bifidobacteria and lactobacilli probiotics. We have used patented and powerful probiotic strains that are not generic imposters. Included in IBtrol we have Bifidobacterium lactis BI-04, Bifidobacterium lactis Bi-07, Lactobacillus acidophilus NCFM, Lactobacillus paracasei Lpc-37, and Bifidobacterium lactis HN019.
Each strain we have included has been rigorously tested in human clinical trials either on its own or in combination with one or more of the other strains we have included here, we hand picked each strain for its health promoting properties and relevance to IBS.
Even more importantly, our exact 5-strain formula has been tested in a large clinical trial of people with IBS (Harris et al 2022) and shown to normalize bowels, reduce pain, protect from infection and improve overall IBS symptoms. In this clinical study 188 people with IBS took part and they used the exact same probiotic formula and dose (12bn CFU per day) that we have included in IBtrol. So you know you are taking the right probiotic backed by science to help improve your symptoms and protect your gut.
Why take all three?

Although each of our three powerful ingredients has shown benefit for IBS symptoms as a stand alone solution, none of the three individual products solves all IBS problems at once. Psyllium reduces gas and normalizes bowel motions but it doesn’t improve the microbiota.
The prebiotic helps improve symptoms and grow beneficial bifidobacteria in the gut but it doesn’t specifically target bowel normalization in the way that psyllium does. The probiotic helps to add more anti-inflammatory strains to the gut, promoting a calmer gut and fostering a healthy gut environment but it doesn’t improve your existing microbiota in the way that Bimuno does. Therefore taking all three together provides a foundation of strength to normalize bowels, improve your microbiome and soothe your gut to protect from flares.
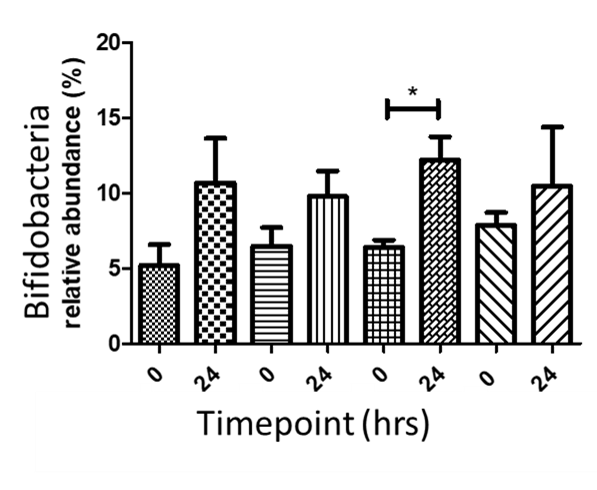
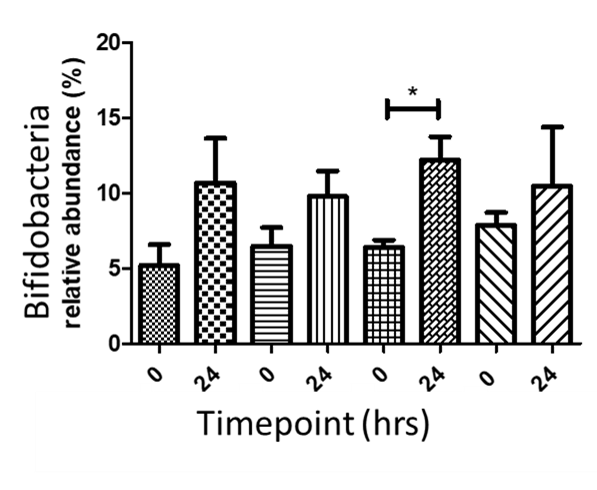
We conducted research using state of the art colon modeling using the human microbiome to ensure that the combination of psyllium with our patented prebiotic did not dampen the effect of the prebiotic. We saw a consistent effect of the prebiotic increasing bifidobacteria (healthy bacteria) when combined with psyllium.
We also examined the effect of adding psyllium to the prebiotic on gas production and saw that the ratio of psyllium to prebiotic we used in our final preparation helped to delay peak gas production, the same effect that has been observed in human MRI studies (REF Gunn et al).
In addition to the colon modeling studies we have conducted a human trial of the psyllium with prebiotic and we saw a reduction in symptoms of pain, flatulence, bloating, heartburn, reflux, burping, hard poo,incomplete bowel motions, and fatigue. The improvement in fatigue and hard poo were significant compared to baseline. In summary, when people took our product they felt they had more energy and had better poop after just four weeks.
We combined the data from our two research studies to select the optimum blend of fibers to have the maximum effect on gut symptoms while improving the microbiome.
Our probiotic has recently been used in a large study of people with IBS (Harris et al 2022). They tested our exact formulation in 188 people with IBS and saw significant improvement in both diarrhea and constipation predominant IBS symptoms over the study.
At Medtrition we are committed to evidence based nutrition, which is why we invested in research studies or used very recent research studies when developing our formula.
- Wilson, Bridgette, et al. "β-Galactooligosaccharide in conjunction with low FODMAP diet improves irritable bowel syndrome symptoms but reduces fecal bifidobacteria." Official journal of the American College of Gastroenterology| ACG 115.6 (2020): 906-915.
- Shepherd, Susan J., et al. "Dietary triggers of abdominal symptoms in patients with irritable bowel syndrome: randomized placebo-controlled evidence." Clinical gastroenterology and hepatology 6.7 (2008): 765-771.
- Cox, Selina R., et al. "Fermentable carbohydrates [FODMAPs] exacerbate functional gastrointestinal symptoms in patients with inflammatory bowel disease: a randomised, double-blind, placebo-controlled, cross-over, re-challenge trial." Journal of Crohn's and Colitis 11.12 (2017): 1420-1429.
- Huaman, Jose-Walter, et al. "Effects of prebiotics vs a diet low in FODMAPs in patients with functional gut disorders." Gastroenterology 155.4 (2018): 1004-1007.
- Hustoft, T. N., et al. "Effects of varying dietary content of fermentable short‐chain carbohydrates on symptoms, fecal microenvironment, and cytokine profiles in patients with irritable bowel syndrome." Neurogastroenterology & Motility 29.4 (2017): e12969.
- Staudacher, Heidi M., et al. "Fermentable carbohydrate restriction reduces luminal bifidobacteria and gastrointestinal symptoms in patients with irritable bowel syndrome." The Journal of nutrition 142.8 (2012): 1510-1518.
- Staudacher, Heidi Maria, et al. "A diet low in FODMAPs reduces symptoms in patients with irritable bowel syndrome and a probiotic restores bifidobacterium species: a randomized controlled trial." Gastroenterology 153.4 (2017): 936-947.
- Wilson, Bridgette, Selina R. Cox, and Kevin Whelan. "Challenges of the low FODMAP diet for managing irritable bowel syndrome and approaches to their minimisation and mitigation." Proceedings of the Nutrition Society 80.1 (2021): 19-28.
- So, Daniel, et al. "Supplementing dietary fibers with a low FODMAP diet in irritable bowel syndrome: a randomized controlled crossover trial." Clinical Gastroenterology and Hepatology 20.9 (2022): 2112-2120.
- Dimidi E, Whelan K. Food supplements and diet as treatment options in irritable bowel syndrome. Neurogastroenterology & Motility 2020;32:e13951.
- Gill, Samantha K., et al. "Dietary fibre in gastrointestinal health and disease." Nature Reviews Gastroenterology & Hepatology 18.2 (2021): 101-116.
- So D, Gibson PR, Muir JG, et al. Dietary fibres and IBS: translating functional characteristics to clinical value in the era of personalised medicine. Gut 2021;70:2383-2394.
- Miller LE, Lehtoranta L, Lehtinen MJ. The Effect of Bifidobacterium animalis ssp. lactis HN019™ on cellular immune function in healthy elderly subjects: systematic review and meta-analysis. Nutrients. 2017;9:191.)
- Pittayanon R, Lau JT, Yuan Y, Leontiadis GI, Tse F, Surette M, Moayyedi P. Gut microbiota in patients with irritable bowel syndrome-A systematic review. Gastroenterology. 2019;157(1):97–13. doi:10.1053/j.gastro.2019.03.049.
- Silk, D. B. A., et al. "Clinical trial: the effects of a trans‐galactooligosaccharide prebiotic on faecal microbiota and symptoms in irritable bowel syndrome." Alimentary pharmacology & therapeutics 29.5 (2009): 508-518.
- Vulevic, Jelena, et al. "Effect of a prebiotic galactooligosaccharide mixture (B‐GOS®) on gastrointestinal symptoms in adults selected from a general population who suffer with bloating, abdominal pain, or flatulence." Neurogastroenterology & Motility 30.11 (2018): e13440.Huaman, Jose-Walter, et al. "Effects of prebiotics vs a diet low in FODMAPs in patients with functional gut disorders." Gastroenterology 155.4 (2018): 1004-1007.
- Harris, Lucinda A., et al. "An open-label, multicenter study to assess the efficacy and safety of a novel probiotic blend in patients with functional gastrointestinal symptoms." Journal of Clinical Gastroenterology 56.5 (2022): 444-451.


Our gut is a wonderful ecosystem with over 100 trillion bacteria making up a large community that works with each other and with our immune system to keep us safe and functioning well.
This microbial community is called our gut microbiome. Irritable bowel syndrome is called a functional gut disorder, because medical tests generally all come back normal but there is still an issue with the way the gut is functioning. This is usually associated with a change in the balance of the gut ecosystem.
The gut microbiome is different in IBS than non-IBS individuals, this is called dysbiosis. The chemical messages created by this imbalanced gut microbiome can affect how quickly the large bowel moves leading to constipation and/or diarrhea as well as altering pain signals to our brain.


Our gut is a wonderful ecosystem with over 100 trillion bacteria making up a large community that works with each other and with our immune system to keep us safe and functioning well.
This microbial community is called our gut microbiome. Irritable bowel syndrome is called a functional gut disorder, because medical tests generally all come back normal but there is still an issue with the way the gut is functioning. This is usually associated with a change in the balance of the gut ecosystem.
The gut microbiome is different in IBS than non-IBS individuals, this is called dysbiosis. The chemical messages created by this imbalanced gut microbiome can affect how quickly the large bowel moves leading to constipation and/or diarrhea as well as altering pain signals to our brain.
Irritable bowel syndrome
is defined as a chronic functional gut disorder and symptoms can include pain, bloating, excess gas and disordered bowel habits, with both unpredictable form and frequency of bowel movements.
IBtrol was developed to
address the symptoms of IBS
but also the underlying dysbiosis of the gut microbiome, helping to foster a balanced gut ecosystem while also managing symptoms of pain, excess gas production and unpredictable bowel movements.
Dr Bridgette Wilson has worked with Medtrition
in the development of IBtrol and with almost two decades of clinical and research experience in IBS, Dr Wilson has ensured that IBtrol is right for all types of IBS. IBtrol includes 3 potent evidence-based components, premium blonde psyllium, GOS-prebiotic and a 5-strain probiotic all at IBS specific doses.

Psyllium
A review of supplements for IBS published in 2020 (Dimidi et al, 2020) found that psyllium improves both abdominal pain and overall symptoms of IBS. A review published in Nature Medicine found that psyllium is useful for normalizing bowel movements in people with IBS with either diarrhea or constipation (Gill et al 2021). Psyllium fiber doesn’t lead to excess gas production when consumed with water, it helps to bulk stool and it binds excess fluid in the gut, making it useful for the treatment of both constipation and diarrhea without worsening IBS symptoms (So et al 2021). 10g of psyllium per day is recommended to see the benefits in IBS.

Prebiotic
Our patented beta-galacto-oligosaccharide (b-GOS) prebiotic is the most extensively researched prebiotic in functional bowel disorders. It has been demonstrated to improve symptoms of IBS in four human clinical trials (Silk et al 2009, Wilson et al 2020, Vulevic et al 2019, Huaman et al 2018). The dose that we have included in IBtrol showed the best effects on IBS symptoms (1.4g of b-GOS per day).

Probiotic
IBtrol combines 5 potent strains of bifidobacteria and lactobacilli probiotics. We have used patented and powerful probiotic strains that are not generic imposters. Included in IBtrol we have Bifidobacterium lactis BI-04, Bifidobacterium lactis Bi-07, Lactobacillus acidophilus NCFM, Lactobacillus paracasei Lpc-37, and Bifidobacterium lactis HN019.
Each strain we have included has been rigorously tested in human clinical trials either on its own or in combination with one or more of the other strains we have included here, we hand picked each strain for its health promoting properties and relevance to IBS.
Even more importantly, our exact 5-strain formula has been tested in a large clinical trial of people with IBS (Harris et al 2022) and shown to normalize bowels, reduce pain, protect from infection and improve overall IBS symptoms. In this clinical study 188 people with IBS took part and they used the exact same probiotic formula and dose (12bn CFU per day) that we have included in IBtrol. So you know you are taking the right probiotic backed by science to help improve your symptoms and protect your gut.

Although each of our three powerful ingredients has shown benefit for IBS symptoms as a stand alone solution, none of the three individual products solves all IBS problems at once. Psyllium reduces gas and normalizes bowel motions but it doesn’t improve the microbiota. The prebiotic helps improve symptoms and grow beneficial bifidobacteria in the gut but it doesn’t specifically target bowel normalization in the way that psyllium does. The probiotic helps to add more anti-inflammatory strains to the gut, promoting a calmer gut and fostering a healthy gut environment but it doesn’t improve your existing microbiota in the way that Bimuno does. Therefore taking all three together provides a foundation of strength to normalize bowels, improve your microbiome and soothe your gut to protect from flares.
We conducted research using state of the art colon modeling using the human microbiome to ensure that the combination of psyllium with our patented prebiotic did not dampen the effect of the prebiotic. We saw a consistent effect of the prebiotic increasing bifidobacteria (healthy bacteria) when combined with psyllium.
We also examined the effect of adding psyllium to the prebiotic on gas production and saw that the ratio of psyllium to prebiotic we used in our final preparation helped to delay peak gas production, the same effect that has been observed in human MRI studies (REF Gunn et al).
In addition to the colon modeling studies we have conducted a human trial of the psyllium with prebiotic and we saw a reduction in symptoms of pain, flatulence, bloating, heartburn, reflux, burping, hard poo,incomplete bowel motions, and fatigue. The improvement in fatigue and hard poo were significant compared to baseline. In summary, when people took our product they felt they had more energy and had better poop after just four weeks.
We combined the data from our two research studies to select the optimum blend of fibers to have the maximum effect on gut symptoms while improving the microbiome.
Our probiotic has recently been used in a large study of people with IBS (Harris et al 2022). They tested our exact formulation in 188 people with IBS and saw significant improvement in both diarrhea and constipation predominant IBS symptoms over the study.
At Medtrition we are committed to evidence based nutrition, which is why we invested in research studies or used very recent research studies when developing our formula.
- Wilson, Bridgette, et al. "β-Galactooligosaccharide in conjunction with low FODMAP diet improves irritable bowel syndrome symptoms but reduces fecal bifidobacteria." Official journal of the American College of Gastroenterology| ACG 115.6 (2020): 906-915.
- Shepherd, Susan J., et al. "Dietary triggers of abdominal symptoms in patients with irritable bowel syndrome: randomized placebo-controlled evidence." Clinical gastroenterology and hepatology 6.7 (2008): 765-771.
- Cox, Selina R., et al. "Fermentable carbohydrates [FODMAPs] exacerbate functional gastrointestinal symptoms in patients with inflammatory bowel disease: a randomised, double-blind, placebo-controlled, cross-over, re-challenge trial." Journal of Crohn's and Colitis 11.12 (2017): 1420-1429.
- Huaman, Jose-Walter, et al. "Effects of prebiotics vs a diet low in FODMAPs in patients with functional gut disorders." Gastroenterology 155.4 (2018): 1004-1007.
- Hustoft, T. N., et al. "Effects of varying dietary content of fermentable short‐chain carbohydrates on symptoms, fecal microenvironment, and cytokine profiles in patients with irritable bowel syndrome." Neurogastroenterology & Motility 29.4 (2017): e12969.
- Staudacher, Heidi M., et al. "Fermentable carbohydrate restriction reduces luminal bifidobacteria and gastrointestinal symptoms in patients with irritable bowel syndrome." The Journal of nutrition 142.8 (2012): 1510-1518.
- Staudacher, Heidi Maria, et al. "A diet low in FODMAPs reduces symptoms in patients with irritable bowel syndrome and a probiotic restores bifidobacterium species: a randomized controlled trial." Gastroenterology 153.4 (2017): 936-947.
- Wilson, Bridgette, Selina R. Cox, and Kevin Whelan. "Challenges of the low FODMAP diet for managing irritable bowel syndrome and approaches to their minimisation and mitigation." Proceedings of the Nutrition Society 80.1 (2021): 19-28.
- So, Daniel, et al. "Supplementing dietary fibers with a low FODMAP diet in irritable bowel syndrome: a randomized controlled crossover trial." Clinical Gastroenterology and Hepatology 20.9 (2022): 2112-2120.
- Dimidi E, Whelan K. Food supplements and diet as treatment options in irritable bowel syndrome. Neurogastroenterology & Motility 2020;32:e13951.
- Gill, Samantha K., et al. "Dietary fibre in gastrointestinal health and disease." Nature Reviews Gastroenterology & Hepatology 18.2 (2021): 101-116.
- So D, Gibson PR, Muir JG, et al. Dietary fibres and IBS: translating functional characteristics to clinical value in the era of personalised medicine. Gut 2021;70:2383-2394.
- Miller LE, Lehtoranta L, Lehtinen MJ. The Effect of Bifidobacterium animalis ssp. lactis HN019™ on cellular immune function in healthy elderly subjects: systematic review and meta-analysis. Nutrients. 2017;9:191.)
- Pittayanon R, Lau JT, Yuan Y, Leontiadis GI, Tse F, Surette M, Moayyedi P. Gut microbiota in patients with irritable bowel syndrome-A systematic review. Gastroenterology. 2019;157(1):97–13. doi:10.1053/j.gastro.2019.03.049.
- Silk, D. B. A., et al. "Clinical trial: the effects of a trans‐galactooligosaccharide prebiotic on faecal microbiota and symptoms in irritable bowel syndrome." Alimentary pharmacology & therapeutics 29.5 (2009): 508-518.
- Vulevic, Jelena, et al. "Effect of a prebiotic galactooligosaccharide mixture (B‐GOS®) on gastrointestinal symptoms in adults selected from a general population who suffer with bloating, abdominal pain, or flatulence." Neurogastroenterology & Motility 30.11 (2018): e13440.Huaman, Jose-Walter, et al. "Effects of prebiotics vs a diet low in FODMAPs in patients with functional gut disorders." Gastroenterology 155.4 (2018): 1004-1007.
- Harris, Lucinda A., et al. "An open-label, multicenter study to assess the efficacy and safety of a novel probiotic blend in patients with functional gastrointestinal symptoms." Journal of Clinical Gastroenterology 56.5 (2022): 444-451.